Table of Contents
V. Complications with Blood Thinners
Blood Loss Prevention
Clotting is the body’s natural way of preventing blood loss when you get a scrape or cut. This process is accomplished by turning liquid blood into a clump of semi-solid blood. Clots that form on an open wound keep the blood inside, but clots that form inside a vein put you at risk of many severe complications.
Well-known complications include heart attack and stroke, but many other conditions may occur because of a blood clot. [1] Typically, people at risk of blood clots may be prescribed Aggrenox (dipyridamole + ASA), Coumadin (warfarin), Elmiron (pentosan polysulfate sodium), or Eliquis (apixaban). Read on to learn about other potential complications of a blood clot.
As the name suggests, deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein. As opposed to surface veins, deep veins run deep within the body. [2] DVT is most commonly caused by blood clots in the legs from long periods of inactivity. Things like sitting in a plane for many hours or being on bed rest after surgery are all factors that can lead to a clot in the legs. To spot DVT, look for symptoms like: If you suspect DVT, you may require medical attention immediately because DVT is often a precursor to a pulmonary embolism (a life-threatening lung complication). [3] A pulmonary embolism (PE) occurs when a blood clot forms in one of the pulmonary arteries in the lungs. DVT often precedes a pulmonary embolism because blood clots in the legs commonly travel to the lungs. Blocked blood flow in the lungs can put your life at risk and requires prompt treatment. You may be having a pulmonary embolism if you are displaying symptoms such as shortness of breath, chest pain, and cough. Other common symptoms of a PE include: The dangers of a PE should not be underestimated. Statistics show that roughly one-third of people with untreated PE do not survive. When a PE and DVT occur simultaneously, it is referred to as venous thromboembolism (VTE). [3] [4] Post-phlebitic syndrome (post-thrombotic syndrome) may occur as a complication if DVT results in venous insufficiency. This is also known as chronic venous stasis. Venous insufficiency is characterized by a reduced blood flow back towards the heart. [5] Post-phlebitic syndrome is a chronic condition that can cause: Post-phlebitic syndrome may develop within weeks or months following a DVT. If you have experienced a DVT recently, you are at risk of developing post-phlebitic syndrome. Compression therapy is often used to treat post-phlebitic syndrome, but medications, topical creams, and surgery are also available options. [7] Many treatment plans involve using blood thinners to manage blood clots. However, some individuals may react adversely to blood thinners. As a result, excessive bleeding may occur and cause: Blood thinners can also increase the risk of internal bleeding. This is why you should promptly visit the hospital after any accidents, no matter how harmless they may seem. Certain foods, herbs, and other medications may also interfere with blood thinners. Telling your doctor about your diet and existing medications will help them prescribe a more effective dosage. [8] Preventing these complications of blood clots starts with eliminating factors that increase your risk. If you must sit for long periods, do ankle rotation exercises to keep your calves active. Your calves play an important role in pumping blood back to the heart. If you are confined to a bed, have an available friend or nurse massage your legs periodically to maintain blood flow. Smoking and being overweight are factors that can increase your risk of blood clots; quitting smoking, eating healthy, and exercising regularly can go a long way in preventing blood clot complications. [4] Talk to your doctor to learn more about treatment options and medications like Aggrenox (dipyridamole + ASA), Coumadin (warfarin), Elmiron (pentosan polysulfate sodium), and Eliquis (apixaban). Keep in mind that blood clots can occur quickly, so you may want to seek medical help if you experience symptoms of a blood clot. The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis, or treatment.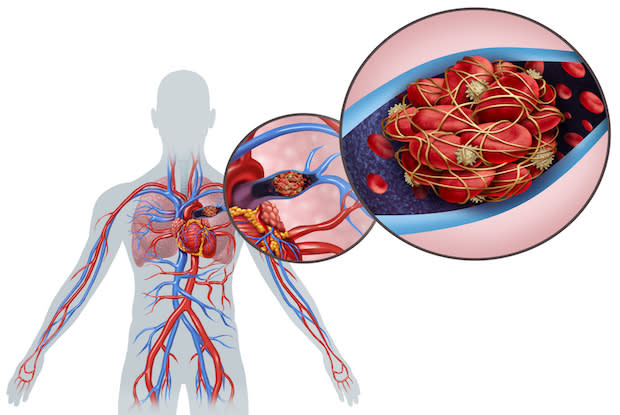
Deep Vein Thrombosis
Pulmonary Embolism

Post-phlebitic Syndrome
Complications with Blood Thinners

Prevention
